Overview of surgical procedures
Basic principles
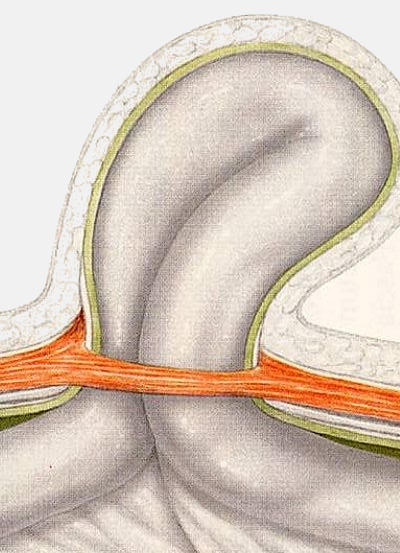
A hernia is the protrusion of tissue through a weak spot in the surrounding wall of the cavity that normally contains it. Because of this opening of the wall, an organ or a part of an organ squeezes through and reaches another region of the body, forming kind of protruding 'sac' (hernia sac).
Several surgical approaches to hernia repair have been developed over the years. All of these different methods follow some basic common principles:
Inversion - Removal
The protruding tissue should get back to where it belongs. To achieve that, surgeons dissect the surrounding tissues and locate the hernia sac and its contents. The hernia sac can be then inverted (pushed or pulled back) or it can be opened and removed (herniotomy).
Closure - Reinforcement
The week spot - opening through which the hernia came out in the first place should be closed and reinforced, in order to remain closed. To achieve that, surgeons can stitch the defect or use a implant to fix the opening as a patch.
FAQ: I have been reading about hernia repair techniques and I am now quite confused. Can you help me understand the differences?
Main differences between hernia repair techniques
The main differences of the various hernia repair procedures can be classified according to the type of:
- surgical approach
- open access (single incision)
- laparoscopic access (multiple very small incisions)
- defect closure
- stitching (herniorrhaphy, tension)
- mesh implant (hernioplasty, tension-free)
- mesh placement
- above the muscle layers (onlay)
- among the muscle layers (inlay)
- below the muscle layers (sublay, preperitoneal)
Layers of the abdominal wall
The layers of the abdominal wall from superficial to deep are:
- Skin
- Subcutaneous tissue
- Muscles
- Peritoneum
Peritoneum
is the membrane that forms the lining of the abdominal cavity, the deepest layer of the abdominal wall just above the intestines
Preperitoneal space
is the space between the peritoneum and the lower surface of the muscles of the abdominal wall
Important facts about hernia repair surgery
Surgical approach: open or laparoscopic
There are 2 surgical approaches in hernia repair surgery: the open and the laparoscopic one.
Open approach
An approach is called open, when the surgeon makes a single incision near the location of the hernia, dissects the surrounding tissues and repairs the hernia under direct vision. The length of the skin incision varies, depending on the chosen open repair technique. An open approach with a very small skin incision is often called mini-open.
"In our center we use both open and laparoscopic approaches for hernia repair, depending on the type and location of each hernia"
Laparoscopic approach
During laparoscopy or keyhole surgery the surgeon makes multiple very small incisions usually slightly away from the location of the hernia. The (abdominal) cavity is then inflated with gas (CO2), which creates the necessary working space for the operation. A thin, lighted tube connected to a camera - monitor system enables the view on the operating field. The dissection of the tissues and the repair of the hernia is done remotely with special long instruments.
Laparoscopically, the hernia repair is performed under general anesthesia with a mesh implant (tension-free) under the muscle layers (sublay).
Inversion or removal of the hernia sac
The protruding hernia tissue should get back to where it originally belongs or at least disappear from the area, it has squeezed into. To achieve that, the surrounding tissues are surgically prepared, in order to locate the protruding hernia sac and its contents. This can be done either open or laparoscopically. The hernia sac can be then inverted (pushed or pulled back) or it can be opened and removed (herniotomy).
"Inversion or removal of the hernia sac is essential during any hernia repair technique"
Closing the hernia defect: stitching or mesh implant
After getting the protruding tissue back to its original location, the surgeon needs to close the defect of the wall, in order to complete the hernia repair. This can be done either by directly stitching the 'hole' or by covering it with a mesh implant, in order to fix it as a patch.
"Depending on the surgical procedure chosen, significant differences in the clinical outcomes can be reported"
Stitching (herniorrhaphy)
The opening of the abdominal wall, where the hernia slided through at the first place, can be directly stitched and closed. A duplication of the muscle fascia can be also used, in order to strengthen the weak area around the hernia defect. No implants are used apart of typical surgical sutures.
However, stitching creates tension, which reduces the blood supply and the healing capability of an already weak muscle. Many studies have shown, that the recurrence rate of hernias repaired using tension was significant higher that hernias repaired tension-free.
"In our center we still use stitching only in children hernia repair and other very special cases"
Mesh implant (hernioplasty)
Instead of closing the hernia defect under tension by stitching it together, a synthetic mesh implant can be used to fix the opening as a patch. This implant is designed as a fine structured mesh, in order to allow the surrounding tissue to grow through and fuse with it. Several mesh materials are used, the most common is polypropylene, which shows an excellent tissue compatibility.
The mesh implant allows a tension-free hernia repair, which provides a significant lower recurrence rate.
"In our center we use mesh for adult hernia repair in most cases"
Mesh implant placement
A mesh implant can be placed above, inside or below the muscle layers. Clinical trials have shown, that the placement of the mesh below the muscle layers (sublay or preperitoneal) seems to provide the best bio-mechanics, while the mesh placement above the muscle (onlay) the worst ones.
"The most important element for a successful hernia repair is the experience of the surgeon performing it"